Feng Gao, MD
- Professor of Medicine
- Member of the Duke Human Vaccine Institute
https://medicine.duke.edu/faculty/feng-gao-md
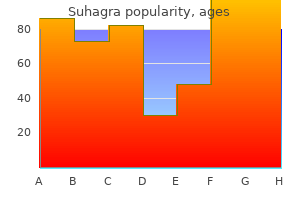
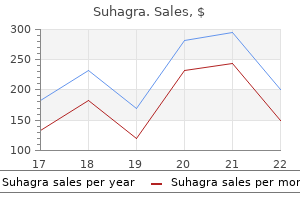
Dengue haemorrhagic fevercan lead to encephalitis or encephalopathy muse erectile dysfunction medication reviews buy discount suhagra 100 mg on-line, transverse myelitis erectile dysfunction ed treatment buy suhagra 100mg lowest price, and mononeuropathy or polyneuropathy similar to that in Guillain-Barre syndrome [20] erectile dysfunction caused by vasectomy suhagra 50mg on line. Enteroviral 71 encephalitis has a high mortality and can present with herpangina or enteroviral hand erectile dysfunction doctors in nc order genuine suhagra on line, foot impotence hypertension discount suhagra 100mg visa, and mouth disease [13] erectile dysfunction juicing purchase suhagra once a day. Complications include myocarditis and acute flaccid paralysis and chronic meningoencephalitis in patients who are immunocompromised [21]. Mumps encephalitis typically starts 3-10 days after parotitis and usually resolves without sequelae, except for occasional hydrocephalus due to ependymal cell involvement [24]. Rabies virus usually incubates for 20-60 days but is capable of incubating for years [29]. Dehydration, respiratory complications, nosocomial infections, and decubitus ulcers may also occur [19]. Focal neurologic deficits (eg, opisthotonos, pareses, tremors, ataxia, hypotonia, diplopia), accentuated reflexes, and extensor plantar responses may be observed [20]. Flaccid paralysis, especially involving the lower extremities, has been described as being due to damage to the anterior horn cells [3]. Enterovirus 71 can cause rhombencephalitis with myoclonus, tremor, ataxia, cranial nerve involvement, neurogenic pulmonary edema, and coma [20]. The availability of antiviral therapy has led to early initiation of the treatment with substantial improvement in the clinical outcome. Some viral encephalitis may be prevented by immunisation (for example, mumps, measles, rubella, Japanese encephalitis, and rabies). Adequate vector control and environmental sanitation are essential to prevent large outbreaks of arboviral encephalitis. Cluster outbreaks of emergence of zoonotic encephalitis continue should be monitor regularly to signal an important public health principle that any new outbreaks of unusual and fatal diseases in animals may herald related events, maybe new infections, in humans. Multipurpose instantaneous microarray Detection of Acute encephalitis causing viruses and their expression profles. Viral aetiologies of acute encephalitis in a hospitalbased South Asian population. Case Defnitions, Diagnostic Algorithms, and Priorities in Encephalitis: Consensus Statement of the International Encephalitis Consortium. Encephalitis Hospitalization Rates and Inpatient Mortality in the United States, 2000 2010. Consensus guidelines for the investigation and management of encephalitis in adults and children in Australia and New Zealand. Viral meningoencephalitis: a review of diagnostic methods and guidelines for management. Viral etiologies in adult patients with encephalitis in Poland: A prospective single center study. Japanese encephalitis associated acute encephalitis syndrome cases in West Bengal, India: A sero-molecular evaluation in relation to clinico-pathological spectrum. Acute non-herpetic viral encephalitis of juvenile onset: analysis of 11 cases based on initial clinical symptoms. Acute Febrile Encephalopathy in Children: A Prospective Study of Clinical Features, Etiology, Mortality, and Risk Factors from Western India. Endemic and emerging acute virus infections in Indonesia: an overview of the past decade and implications for the futur. Days 2-3, she exhibited slowing speech, confabulation and confusion with halting speech and possible hallucinations. Mortality Secondary to Hyperemesis Gravidarum: A Case Report Page 2 of 7 Week 10:The following day, her husband found her incoherent imbalance. She was hypertensive, emaciated, disoriented, via a percutaneous endoscopic gastrostomy tube. On day and acyclovir were administered until infectious and autoimmune 36, the patient had respiratory failure. Week 11: Due to inability to move, paucity of speech, Mental status changes are nearly universal and exhibited as brisk reflexes, clonus, hyperesthesia, and somnolence, she was dizziness, drowsiness, apathy, and cognitive impairment [46,52]. Tachycardia with atrial arrhythmias and dysphagia noted: elevated transaminase levels, diffuse background slowing continued. Unfortunately Neurology noted pathologically brisk reflexes in her upper for this patient, antibiotics and nutritional intervention were not extremities and lower extremity withdrawal, thus concluding initiated for two weeks. Achieving normonatremia is crucial as the presence of even high carbohydrate diet [61,66], coexisting deficiencies. Mg) mild hyponatremia increases mortality risk by 30%, regardless of [56,66], limited food variety, prolonged malnutrition, impaired comorbid conditions [83]. Further, thiamin testing normonatremia, only to develop persistent dysarthria and is not always available or reliable, and researchers report 50% of dysphagia before becoming comatose and hyponatremic. Clinicians postulated her acids for their production, thus increasing the probability of symptoms were an eating disorder or psychosis, and suggested demyelination [78,88,89]. Beginning pre-hospitalization, however, her neurological symptoms impaired self-feeding. Proactive and more not given immediately, it might be delayed or never given systematic intervention with nutritional therapy and electrolyte [56,103]. We, therefore, continue to recommend concurrent replacement would have improved the odds for this patient and administration [45]. Delayed diagnosis in addition to inadequate treatment and nutritional Finally, we recommend serum electrolytes be checked on intervention resulted in her death. Careful replenishment and thyroid storm, dehydration, and/or severe thyrotoxicosis. In ongoing monitoring should be performed regularly until patients addition to our case, these fatalities illustrate the importance are asymptomatic with adequate intake. Maternal Wt loss <5% Rehydrate**, evaluate needed lifestyle & antiemetic changes. Wt loss >10% Rehydrate**, run comprehensive labs to determine nutritional Recommendations status, give parenteral vitamins including B complex daily, reevaluate antiemetic strategy & tolerability, consult with nutritional support regarding Firstly, we recommend documentation and investigation increasing protein and vitamins, esp. Additional nutrients such as vitamin K [108], zinc, selenium, iron, Secondly, we recommend prescribing prenatal vitamins magnesium and calcium are likely defcient; replenishment benefts mother and which contain a minimum of 5 mg of thiamin to all pregnant baby and may preempt additional complications [109,110]. Protocols should recommend Malabsorption [38,114] infusing thiamin up to 1000 mg/day daily for 5 days to 3 weeks Antibiotics [115] to replenish stores [42,51,53,56,82], or until oral intake resumes. Glucose Infusion [53] Recent studies suggest it is not critical that thiamin be Anemia [106] infused simultaneously with glucose [102]. Mortality Secondary to Hyperemesis Gravidarum: A Case Report Page 5 of 7 Education Complicated by Hyperemesis Gravidarum. Wernicke encephalopathy after Roux en-Y gastric bypass and hyperemesis gravidarum. Pneumomediastinum following esophageal rupture associated with hyperemesis gravidarum. Prenatal exposure to hyperemesis New Zealand Journal of Obstetrics and Gynaecology. Hyperemesis Gravidarum is a Syndrome of Metabolic and Endocrine Disturbances: A Case Description. Hyperemesis gravidarum complicated by Wernicke encephalopathy: background, case 72. Comprehensive Review of the Relative Clinical and intractable vomiting: the role of dual thiamin and corticosteroid therapy. Utility of B-Type Natriuretic Peptide and N-Terminal Pro-B-Type Natriuretic Case Reports in Neurological Medicine. Akinetic-rigid syndrome due to extrapontine and pontine 1):bcr2013009648-bcr2013009648. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. Akinetic mutism in Wernicke-Korsakoff disease: a case 2004;75(suppl 3):iii22-iii28. Nagler E, Vanmassenhove J, van der Veer S, Nistor I, Van Biesen W, Webster infant death syndrome. Locked-in Syndrome due to Central Pontine Myelinolysis: of vitamin-free parenteral nutrition. Renard D, Castelnovo G, Campello C, Bouly S, Le Floch A, Thouvenot E, et a literature review. Thiamin tetrahydrofurfuryl disulfde improves energy metabolism and physical performance during physical 89. A Case of Maternal Vitamin K Defciency Associated with Hyperemesis Gravidarum: Its Potential 93. Imaging-based Recurrence of Hyperemesis Gravidarum across generations: population diagnosis of Wernicke encephalopathy: a case report. Cirrhotic cardiomyopathy may be masked by the typical high cardiac output and low pe ripheral vascular resistance often found in liver failure. Portopulmonary hypertension and hepatopulmonary syndrome often found with liver cirrhosis are at opposite ends of a vascular endothelial dysfunction pathway. The hepatic artery provides 25% and the portal vein provides 75% of the blood supply. Bile canaliculi, between hepatocytes, form into bile ducts that drain into the intestine. Disclosure Statement: None of the authors have financial disclosures related to this article. Glucose is stored as glycogen and is converted by the liver to lactate, with the generation of energy. Another important liver function is drug metabolism, espe cially via the cytochrome p450 isoenzymes. The etiologies of the liver disease that most frequently need transplantation are listed in Box 1. Given the new effective antiviral therapies for hepa titis C virus and the increasing obesity epidemic, nonalcoholic fatty liver disease is likely to become the most common cause of liver disease in the United States in the future. Hepatocellular death can occur via necrosis or apoptosis, most often owing to ischemia, viruses, and drug and alcohol toxicity. Cirrhosis refers to the damaging effects of inflammation, hepatocellular injury, and the resulting fibrosis and regeneration of the liver, all of which result in loss of normal liver function. Increased resistance to blood flow through the liver leads to portal hypertension and the development of varices. Higher waitlist priority is also given to patients with certain disease processes, such as acute liver failure, pri mary nonfunction of a recently transplanted liver, and hepatocellular carcinoma. Rules regarding scoring and exception points are changing to attempt to address inequities in access. This committee includes surgeons, hepatologists, anesthesiologists, and social workers. They focus on medi cal comorbidities, functional status, and a psychosocial evaluation. In the United States alone, 40,000 patients die of liver disease each year, but only 6000 liver trans plants are performed annually.
Bacterial meningitis in increased intracranial pressure due to brain tumor erectile dysfunction raleigh nc purchase discount suhagra line, with a review the United States in 1995 erectile dysfunction drugs walmart buy suhagra 50 mg online. Community a study of 129 patients with papilledema or intracranial acquired bacterial meningitis in adults erectile dysfunction treatment pakistan purchase suhagra overnight delivery. Worldwide Haemophilus inuenzae type b disease at the 34 van Crevel H erectile dysfunction agents buy cheapest suhagra, Hijdra A erectile dysfunction medicine online discount generic suhagra canada, de Gans J erectile dysfunction treatment in egypt suhagra 50 mg lowest price. Eect of introduction of tomography of the head before lumbar puncture in adults with the pneumococcal conjugate vaccine on drug-resistant Streptococcus suspected meningitis. Clinical recognition of meningitis in adults: new approaches to management and meningococcal disease in children and adolescents. The rational clinical pediatric bacterial meningitis: dening the time interval for examination. Ten years of clinical Children with meningeal signs: predicting who needs empiric experience with adult meningitis at an urban academic medical antibiotic treatment. A of a multivariable predictive model to distinguish bacterial from 12-year review. Cerebral herniation during for dierentiating bacterial from viral meningitis in infants and bacterial meningitis in children. Recent survey of infectious meningitis mechanisms mediating injury and recovery in the nervous system. Community-acquired Drug insight: adjunctive therapies in adults with bacterial bacterial meningitis: risk stratication for adverse clinical outcome meningitis. Early treatment of low doses of hydrocortisone and udrocortisone on mortality in meningococcal disease. Inuence of given before admission in reducing mortality from meningococcal dexamethasone on ecacy of ceftriaxone and vancomycin therapy disease: systematic review. Bactericidal activity against Prospective international registration of patients may be needed. Dexamethasone aggravates hippocampal apoptosis and learning Antibiotic guidelines and antibiotic use in adult bacterial deciency in pneumococcal meningitis in infant rats. The penetration of anti-infectives into the diagnosis, investigation, treatment and prevention of acute bacterial central nervous system. Dexamethasone as multidrug-resistant Streptococcus pneumoniae in the United States. Received: March 15, 2018; Published: April 05, 2018 Abstract Background: Bacterial meningitis remains a major cause of morbidity and mortality in childhood worldwide. Diagnosis of bacterial meningitis is challenging, as clinical and laboratory findings are not always present and often have limited diagnostic accuracy. Aims: To summarize salient features on diagnosis and treatment of bacterial meningitis in children and identify challenges currently faced in the era of conjugate vaccines. Results: Although the incidence of bacterial meningitis has significantly decreased following the introduction of conjugate vaccines, new challenges have arisen, with change of serotype distribution and shift of the disease burden to neonatal and early infantile pe riod. Conclusions: Future perspectives have to turn on further development of conjugate vaccines, that should target all strains regardless of their capsule type, as well as focus on neonatal and maternal immunization. Haemophilus influenzae type b (Hib) was the major cause of paediatric meningitis, before the introduction of Hib vaccines [2]. The classic signs and symptoms include fever, vomiting, altered mental status, anorexia, petechial rash, convulsions, headache and photophobia. In infants, bulging fontanelle, pale or marble skin, poor feeding and irritability may be the first signs and symptoms, whether in older children classic signs of neck stiffness, Kerning and Brudzinski are not always present. In the adult population, sensitivity of these signs is only 5% for both of them, while this is approximately 30% for nuchal rigidity [3]. Meningitis is confirmed with laboratory tests in only 11-30% of children with meningeal signs [4,5], while these signs can be absent in 20% of paediatric meningitis cases [6]. Cervical lymphadenitis and pleural irritation due to pneumonia may also provoke meningeal signs in the absence of meningitis [6]. A lumbar puncture is necessary for the definitive diagnosis of bacterial meningitis. However, established criteria can identify the high risk patients, that need antibiotic therapy even before a lumbar puncture is performed [4]. Latex agglutination is a rapid method for the etiological diagnosis of bacterial meningitis, but it has a variable sensitivity rate (22% to 100%), which can be decreased after antibiotic treatment, dependent on the causative microorganism [14]. Hospital antibiotic therapy, on the other hand, is recommended within the 1sthour after admission and not > 3 hours after the contact with a health service [21,22]. In any case, blood cultures need to be collected before the first dose of antibiotic therapy [21]. Alternatively, amoxicillin or ampicillin plus an aminoglycoside can be used for neonates [7,11]. After identification of the pathogen, antibiotic therapy can be modified according to the susceptibility patterns. For acute meningitis due to penicillin-sensitive Streptococcus pneumoniae, penicillin or ampicillin/amoxicillin for 10 14 days is acceptable, although not pref erable for most clinicians in a developed world setting due to the frequency of required administration 4 hourly for penicillin in menin gitis. In case of reduced susceptibility of Streptococcus pneumoniae, ceftriaxone or cefotaxime should be combined with either vancomycin or rifampicin [7]. Bacterial meningitis by Neisseria meningitides can be treated with penicillin/amoxicillin/ampicillin if it is penicillin Citation: Fani Ladomenou. Therapeutic options for Haemophilus influenzae type B meningitis include ceftriaxone or cefotaxime for 7 to 14 days, while Listerial meningitis requires ampicillin or amoxicillin for 21 days, in combination with gentamicin for the first 7 to 10days [21]. In case of staphylococcal meningitis, antibiotic therapy should last for at least 14 days and should include flucloxacil lin, nafcillin or oxacillin for methicillin sensitive bacteria, vancomycin for resistant to methicillin and linezolid for vancomycin-resistant Staphylococcus aureus [7]. For Gram negative Enterobacteriaceae, cefotaxime, ceftriaxone or meropenem are recommended for 21 to 28 days, whereas bacterial meningitis without identification of the responsible microbial strains should be treated for at least 10 to 14 days [21]. In patients with known history of severe beta-lactam allergy, vancomycin can be administered as the alternative for pneumococcal or staphylococcal meningitis, chloramphenicol for meningococcal and cotrimoxazole for listerial meningitis [21]. Meropenem can be used for the empiric therapy of inpatients with community-acquired bacterial meningitis that are allergic to penicillin or for hospital-acquired bacterial meningitis combined with vancomycin [24]. Linezolid acts only in Gram positive bacteria, has been used for multi-resistant microorganisms and should only be used after resistance tests recommend it [24]. This is clinically relevant since some pneumococcal strains may be penicillin resistant S. Dexamethasone can moderate the harmful response caused by the proinflammatory mediators that are produced when antibiotics interact with bacteria [27]. It has also been proposed that glucocorticoids acting with Toll-like receptors promote anti-inflammatory and immunosuppressive response [28]. Treatment with dexamethasone should be started ideally before or with the first dose of antibiotics [11] while the European guidelines suggest that a delay of up to 4 hours after the initia tion of antibiotic therapy is acceptable [7]. Regarding the duration of dexamethasone therapy, European guidelines recommend a total duration of 4 days in case of pneumococcal and Hib meningitis in children [7,21] whereas American guidelines recommend the use of dexamethasone for 2 4 days in children with Hib meningitis. Other adjunctive therapies the use of osmotic agents, such as mannitol or hypertonic saline, has been proposed to reduce intracranial pressure, but they are not recommended for children with bacterial meningitis as there are not sufficient data to prove favorable outcome. On the other hand, glycer ol and therapeutic hypothermia should not be used in bacterial meningitis, as increased mortality has been associated with their use [7]. The impact of conjugate vaccines Conjugate vaccines, comprising a conjugate between an antigenic protein and a polysaccharide, have been developed against a variety of bacterial species to overcome the issues associated with the T cell-independent immunological characteristics of pure polysaccharide antigens [29]. In particular, a conjugate vaccine, depending on T cell dependent response, is expected to have benefits over a polysac charide vaccine, in terms of booster response, immunological memory and generally improved immune responses, due to the T cell dependent characteristics of the immune response. Thus, immunological memory is established and herd immunity effect is enhanced with the use of conjugate vaccines [30]. Conjugate vaccines have been developed against the main causes of paediatric meningitis in the past; pneumococcal, meningococcal serotypes and Hib. These young infants are dependent on indirect (herd) protection, and thus, delayed vaccine impact in this population could be expected [33]. To overcome this problem, new vaccines covering more serotypes including the emerging serotypes have been developed. However, no significant results were found in the hospital course or outcome, except the greater percentage of patients with subdural empyema and hemiparesis [35]. This is due to the processes of selec tion and recombination that play a critical role in the emergence of multi-resistant strains and the serotype replacement, which leads to change of serotype distribution, most frequent in serotypes before the vaccine implementation. We thus expect that the long-term use of multi-valent conjugate vaccines will contribute to serotype replacement, unless the formulation could contain all capsular types. Another way to solve this problem of serotype replacement would be to develop new types of vaccines, that will target any pneumococcal strain regardless of its capsule type [38]. Overall 13 serotypes of the meningococcus have been isolated, with only five of them associated with invasive disease (A, B, C, Y, X and W135) [39]. Four of the disease-causing serogroups (A, C, Y, and W) can be effectively prevented with available quadrivalent capsular polysaccharide protein conjugate vaccines; however, capsular polysaccharide conjugate vaccines are not effective against meningococcal serogroup B (MenB) and there is no vaccine available for serogroup X. After the implementation of MenC vaccination program, disease incidence and mortality by serogroup C have dramatically declined and this effect has been reported in both vaccinated and unvaccinated children [40,41]. However, the challenges of MenC and the rest of the conjugate meningococcal vaccines consist of the duration of protection provided and the need of repeated booster doses to provide continuing protection [42]. Meningococcal disease is hyperendemic in this region, and periodic epidemics Citation: Fani Ladomenou. Bacterial Meningitis in Childhood: Diagnosis, Management and Challenges in the Era of Conjugate Vaccines 385 during the dry season (December June) reach up to 1,000 cases per 100,000 population. Historically, outbreaks in the meningitis belt were primarily due to serogroup A and this led to the introduction of a new conjugate vaccine against group A serotype (MenAfriVac) in the African meningitis belt in 2010. MenA conjugate vaccine is more immunogenic than the previously mentioned conjugate meningococ cal vaccines as it eliminates the carriage of group A meningococcus throughout vaccinated and unvaccinated individuals [41]. However, with the introduction of MenAfriVac in this region, recent meningococcal outbreaks have primarily been due to serogroups C and W, although serogroup X outbreaks are also reported. This could be attributed not only to the direct protection of the vaccine, but also to the lower carriage of Hib in the nasopharynx of children, offering herd immunity [45]. However, nowadays, more than two decades after the implementation of the Hib conjugate vaccine, the epidemiology of invasive H. With more countries implementing Hib conjugate vaccines, it will be timely to set up better surveillance network to document any changing epidemiology that may occur upon introduction of vaccines targeting infections with multiple antigenic variants. Conjugate vaccines and neonates the first days of life are prone to infections due to the unique nature of the neonatal immune system, which is a direct consequence of the challenging immunological adaptation during the transitional period from intra to extrauterine life. The World Health Organization estimates that 45% of deaths among children under the age of 5 years occur during the newborn period [48]. The interest for conjugate vaccines has now been focused on neonatal vaccination, which could potentially provide early protection for newborns and infants, narrowing the critical period of vulnerability intrinsic to routine vaccination schedules that start later in life. In both studies, the safety profile was reassuring and good respons es to the vaccine administered at birth were documented [50]. However, there was no evidence of hampering potential long-term protec tion or inducing immune tolerance [51]. A variety of approaches have been proposed to overcome the inherent regulatory constraints of the newborn innate and adaptive immune system, including alternative routes of delivery, novel vaccine configurations, improved innate receptor agonists and optimized antigen-adjuvant combinations [50,51]. Maternal immunization could be an alternative choice for infant protection, as prevention of severe infections has been proposed without adverse effects [50]. Further clinical trials are currently underway or being planned to examine both maternal and neonatal pneumococcal-conjugate vaccination in low-income settings [52]. In order to develop improved neonatal vaccines, better and more ap plicable research models will be required; this would enable the accurate assessment of both vaccine immunogenicity and safety [51]. Conclusions Despite the introduction of new antibiotic agents and new types of vaccines, bacterial meningitis remains a major cause of morbidity and mortality in childhood worldwide. Although the incidence of bacterial meningitis has significantly decreased following the introduc tion of conjugate vaccines, new challenges have arisen, with change of serotype distribution and shift of the disease burden to the neona tal and early infantile period. Thus, new conjugate vaccines are needed that would target all strains regardless of their capsule type. More over, research should focus on maternal and neonatal immunization, targeting the age with the main burden of the disease at the moment. Bacterial Meningitis in Childhood: Diagnosis, Management and Challenges in the Era of Conjugate Vaccines 386 Source of Support None. Meningitis (bacterial) and meningococcal septicaemia in under 16s: recognition, diagnosis and management. Bacterial Meningitis in Childhood: Diagnosis, Management and Challenges in the Era of Conjugate Vaccines 387 17. Bacterial Meningitis in Childhood: Diagnosis, Management and Challenges in the Era of Conjugate Vaccines 388 36. Interpreter / cultural needs Infection may occur at the needle site, and affect the bones of the back or the spinal fluid. Yes No Local problems from needle injury are uncommon A Cultural Support Person is required Yes No and include occasional implantation of skin cells that can cause local lumps or tumours (dermoids).
Heparin with and without grad deep vein thrombosis in patients with malignant dis ed compression stockings in the prevention of throm ease erectile dysfunction shake recipe buy generic suhagra 100mg online. Surg Gynecol venous thrombosis in patients with intracranial disease Obstet 1991;172:44-8 erectile dysfunction drugs sublingual suhagra 50mg on line. Prevention of deep vein thrombo matic compression alone for prevention of venous sis in urological patients: a controlled impotence at 37 50mg suhagra with amex, randomized trial thromboembolism after abdominal surgery: a rand of low-dose heparin and external pneumatic compres omized erectile dysfunction pills not working discount 100mg suhagra fast delivery, double-blind comparison erectile dysfunction treatment center buy cheap suhagra 100mg on line. The effcacy of pneumatic sis in neurosurgical patients: a controlled erectile dysfunction nutrition buy discount suhagra 50 mg on line, randomized compression stockings in the prevention of pulmonary trial of external pneumatic compression boots. Improved hemodynamic effectiveness and for prevention of deep venous thrombosis in general associated clinical correlations of a new intermittent abdominal surgery. Inhibition of tissue factor pathway during pression in patients with gynecologic malignancy. Ob intermittent pneumatic compression: A possible mech stet Gynecol 1984;63:92-8. Current practices in the prophylaxis therapy in postoperative and posttrauma patients: a of venous thromboembolism in bariatric surgery. Prevention of postoperative leg prophylaxis in morbidly obese patients undergoing vein thrombosis by electrical muscle stimulation. Effcacy of extended intravenous heparin infusion prevents peri-operative thrombo-prophylaxis in major abdominal surgery: thromboembolic events in bariatric surgery patients. Arch Intern Med study of the time period of venous thromboembolism 2002;162:1245-8. A clinical study with 125I-fbrinogen and pul course of postoperative venous thromboembolism: monary scanning. Arch Surg plications in cancer patients after surgery: a role for 1997;132:499-504. The presence of additional risk factors indicated in the text is likely to increase the risk of thromboembolism for individual patients. Occurrence and Two small randomized studies involving 153 course of thrombosis following prostatectomy. Acta Radiol Diagn (Stockh) patients undergoing open urological procedures 1970;10:513-33. Prophylaxis of post 6-8, 10-22 A study of 579 patients having radical operative leg vine thrombosis by low dose subcutaneous heparin or peroperative calf muscle stimulation: a con prostatectomy did not fnd any difference in trolled clinical trial. Prevention of postoperative deep-vein thrombosis by low-dose heparin in urological surgery. Prevention of deep vein thrombo patients having transurethral resection are not sis in urological patients: a controlled, randomized trial available. Prophylaxis of postoperative ve Recommendations nous thrombosis in a controlled trial comparing dextran 70 and low-dose heparin. Incidence of symp in prostate cancer patients undergoing laparoscopic or tomatic venous thromboembolism after different elec robot-assisted laparoscopic radical prostatectomy. Complications of 2,775 uro boembolic complication rate after radical retropubic logical laparoscopic procedures: 1993 to 2005. Venous afford long-term prophylaxis against deep vein throm thromboembolism in radical prostatectomy: is hepari bosis in urological patients. Progestogen-only oral be minimal for benign laparoscopic gynecologic contraceptives need not be discontinued even surgery,8 and as high as 16% in surgery for ovar when immobilization is expected. The puerperium is associated with a higher frequency of bleeding the time of greatest risk, with a twenty-fold in 33 crease. Weight (kg) Enoxaparin Dalteparin Tinzaparin (75u/kg/day) <50 20mg daily 2,500units daily 3,500 units daily 50-90 40mg daily 5,000 units daily 4,500 units daily 91-130 60mg daily* 7,500 units daily* 7,000 units daily* 131-170 80mg daily* 10,000 units daily* 9,000 units daily* >170 0. This assessment should be tally and throughout the six weeks postpartum repeated if the woman is admitted to a hospi (level of evidence: moderate). Reports have shown that a once-daily longer present and no known thrombophilia or dosage of tinzaparin provides adequate 24 hour additional risk factors should be offered ante cover. The subcutaneous injections should be given in Women with no personal history of venous the fank well away from the incision to minimize thrombosis but who have a thrombophilic de wound hematoma. All should be offered anticoagu ean section (particularly an emergency proce lant prophylaxis following delivery. The risk of dure during labor), gross varicose veins, pre thrombosis should be discussed with the pa eclampsia, postpartum hemorrhage (>1000 mL) tient antenatally and GeC stockings should and immobilization (level of evidence: low). Aspirin is discontinued at 36 risk, prophylaxis should continue for 5-7 days, weeks gestation to allow fetal platelets to recover. Low doses of subcutaneous heparin in the prevention of deep vein thrombosis after gy 1. Epidemiology, risk factors and prophylaxis of venous thrombo-embolism in obstetrics and gynaecol naecological surgery. Acta Chir Scand Suppl weight heparin in gynecologic oncology surgery: a rand 1977;478:1-120. Venous thromboembolism prophylaxis high risk of deep venous thrombosis after elective major in gynecologic oncology: a prospective, controlled trial abdominal surgery. J Thromb Haemost heparin regimens for the prevention of postoperative 2007;5:503-6. Ovarian cancer and venous throm sus unfractionated heparin for prevention of deep boembolic risk. Low dose heparin versus low molec venous thromboembolism in women using oral contra ular weight heparin (Kabi 2165, Fragmin) in the proph ceptives with differing progestagen components. Hormone replacement therapy and cologic oncology: report of a randomized controlled venous thromboembolism. A randomized trial of low-dose ciation of oral and transdermal oestrogen-replacement heparin and intermittent pneumatic calf compression therapy with venous thromboembolism risk. The effcacy of gradu against venous thromboembolism with enoxaparin af ated compression stockings in the prevention of deep ter surgery for cancer. Ann Intern Med lar-weight heparin for obstetric thromboprophylaxis: 2005;143:697-706. Safety of withholding heparin in nous thromboembolism during pregnancy and the post pregnant women with a history of venous thromboem partum period: incidence, risk factors, and mortality. J Thromb Haemost in the risk for recurrence during pregnancy in women 2008;6:905-12. Tinzaparin sodium for thrombosis treatment and without antithrombotic prophylaxis. Risk of pregnancy-asso molecular weight heparin (tinzaparin) therapy for mod ciated recurrent venous thromboembolism in women erate risk thromboprophylaxis during pregnancy. New York: ternational, retrospective study of the safety and effcacy Marcel Dekker; 2003. Blanco-Molina A, Trujillo-Santos J, Criado J, Lopez L, phospholipid antibodies (or antiphospholipid antibod Lecumberri R, Gutierrez R et al. Wu O, Robertson L, Twaddle S, Lowe G, Clark P, Walker antibody or lupus anticoagulant. The phar Conference on Antithrombotic and Thrombolytic Ther macologic basis of therapeutics. A study of pulmonary heparins for thromboprophylaxis and treatment of ve embolism and deep leg vein thrombosis after major gy nous thromboembolism in pregnancy: a systematic re naecological surgery using labelled fbrinogen-phlebog view of safety and effcacy. Ini boprophylaxis but the greater is the risk of tial European experience suggested that neurax bleeding complications. However, if a given dose of the drug is administered ride) can be given safely four hours after removal too long before surgery, then, intra-operative of the epidural catheter (see section on pregnan blood levels would be inadequate for effec cy). This that postoperative administration of the agent is should reduce the risk of surgical bleeding, generally safer and more predictable than preop yet intraoperative thrombogenesis is not pre erative administration when epidural analgesia vented and thrombi may have already begun is needed. Therefore, prophylaxis needs to be given close but not Duration of prophylaxis in too close to surgery. Incidence Isolated lower limb injuries Hjelmstedt and Bergwall, 196894 76 34 Abelseth et al. The optimal duration of prophylaxis is frequency of venographically detected total unknown. Furthermore, national drug registries have However, this was at the expense of a slight in shown warfarin to be a major cause of readmis crease in hemorrhagic complications. Two large rand are few robust studies specifc to orthopedic sur omized controlled trials compared fondaparinux gery. Direct comparisons with for 35 days after surgery, followed by bilateral chemical prophylaxis are sparse; there is proba venographic studies. In a double blind placebo controlled study dian 33 days) when bilateral venography was Vol. There was no signifcant (c) electiVe Knee replAcement difference in major bleeding events between the risk the various groups in either study. However, major In the frst study, the overall rate of primary bleeding was more common with fondaparinux events was much lower than anticipated (pri (2. This increased rate of mary effcacy outcome 9% with apixaban and bleeding with fondaparinux was driven by a mi 8. Two double-blind non-inferiority tri involved 2531 evaluable patients, both prophy als evaluated the effcacy and safety of dabigat lactic regimens were given for 10-14 days. Among 1896 patients, dabigatran 220 and 110 mg showed inferior ef the effect of extending prophylaxis using fcacy to enoxaparin (P=0. There was no signifcant difference in major bleeding events between the various Recommendations groups in either study. In the second study involving 277 considered in all cases (level of evidence: high). In a second study, patients who received hip or knee arthroplasty (4088 patients), as fondaparinux for seven days were randomized to pirin in a dose of 160 mg daily started preop continuation with fondaparinux or placebo for eratively was used as the primary prophylactic a further three weeks. There was no difference in hem ever, universal prophylaxis would be very expen orrhagic complications. None of the new oral anticoagulant regimens shown to be effective in elective hip and knee re prophylactic methods and recommendations placement, have been tested in the hip fracture population. Ad 2-3) (level of evidence: high) or lDuh (level verse effects were more frequent in the inter of evidence: high). The cumulative incidence of major or (e) Knee ArthroScopy clinically relevant bleeding events was 0. This poses ditional risk factors or when extensive surgery a dilemma: rare events in a common procedure beyond a simple diagnostic procedure is per will lead to quite a high number of events even formed. More effective methods are needed in (F) iSolAteD BeloW Knee well-defned groups of patients. The prophylactic methods and recommendations drug will need to be administered in the outpa tient setting until the patient is weight bearing. General considerations this group is so heterogeneous that studies (G) multiple trAumA and recommendations are diffcult to devise. A clinical risk assessment is mandatory and for the risk those with risk factors, safe prophylaxis must be instituted. Well-designed studies in this area are few and electrical stimulation of the calf muscles thromboprophylaxis has to be assessed accord may be considered in patients in whom pharma ing to the risk for bleeding. Thus, me General considerations chanical methods are attractive if chemical prophylaxis is contraindicated. Timing of initial administration of low prophylactic methods molecular-weight heparin prophylaxis against deep vein thrombosis in patients following elective hip and recommendations arthroplasty: a systematic review. The effectiveness of General considerations intermittent plantar venous compression in prevention of deep venous thrombosis after total hip arthroplasty. It appears minimal risk of hemorrhage resulting from thrombo sis prevention in regional anesthesia]. Lakartidningen that patients with spinal cord injury are not only 1992;89:4028-30. Central neuraxial block and low mo lecular weight heparin (enoxaparine): lessons learned group to prophylactic measures. A to prevent venous thromboembolism after primary hip series of 1162 cases with no routine chemical prophy or knee replacement. Arch In oral anticoagulants after total hip arthroplasty: a pro tern Med 1998;158:1525-31. Embolic complications of calf throm son of low-molecular-weight heparin with oral antico bosis following total hip arthroplasty. Incidence of posthospitalization short-term enoxaparin for the prevention of venous proximal deep venous thrombosis after total hip arthro thromboembolism after total hip arthroplasty: a double plasty. Rivaroxaban versus enoxaparin tern, described by a scoring of the thrombotic burden. Mortality after total hip replacement: 0-10-year fol lism after total hip replacement. Fatal vascular outcomes following major replacement: double-blind randomised comparison of orthopedic surgery. Subcutaneous ancrod in prevention of hospitalization and three months after discharge. The effcacy of prophylaxis with boembolism after elective and post-traumatic hip sur low-dose warfarin for prevention of pulmonary embo gery a controlled prophylactic trial with dextran 70 lism following total hip arthroplasty. Low-molecular-weight heparin cess of high doses of heparin during total hip replace prophylaxis using dalteparin extended out-of-hospital ment for osteoarthritis]. Nouv Presse Med 1974;3:1317 vs in-hospital warfarin/out-of-hospital placebo in hip 9. Prevention of thromboembolic dis prospective, randomised, placebo-controlled study with ease after elective surgery of the hip. Deep vein thrombosis following total hip replacement by vein thrombosis following total knee replacement.
The recommended dose of furosemide is 1 mg/kg for infants during the first year of life erectile dysfunction muse suhagra 50 mg mastercard, while 0 erectile dysfunction natural order discount suhagra online. However impotence libido order suhagra now, it should be borne in mind that reflux has been detected in up to 25% of cases of prenatally detected and postnatally confirmed hydronephrosis [687] erectile dysfunction treatment side effects order on line suhagra. The prognosis is hopeful for a hydronephrotic kidney zyrtec impotence suhagra 100mg discount, even if it is severely affected treatment erectile dysfunction faqs purchase suhagra 100 mg with visa, as it may still be capable of meaningful renal function, unlike a severely hypoplastic and dysplastic kidney. It is important to be able to tell the caregivers exactly when they will have a definitive diagnosis for their child and what this diagnosis will mean. In some cases, however, it will be immediately obvious that the child is severely affected; there will be evidence of massive bilateral dilatation, bilateral hypoplastic dysplasia, progressive bilateral dilatation with oligohydramnios, and pulmonary hypoplasia. Intrauterine intervention is rarely indicated and should only be performed in well-experienced centres [691]. The most commonly used antibiotic in infants with antenatal hydronephrosis is trimethoprim, but only one study reported side effects [692]. Continuous antibiotic prophylaxis should be reserved for this sub-group of children who are proven to be at high risk. In experienced hands, laparoscopic or retroperitoneoscopic techniques and robot-assisted techniques have the same success rates as standard open procedures. Well-established benefits of conventional laparoscopy over open surgery are the decreased length of hospital stay, better cosmesis, less post-operative pain and early recovery [696, 697]. There does not seem to be any clear benefit of minimal invasive procedures in a very young child but current data is insufficient to defer a cut-off age. Data suggest that children with a ureteric diameter of > 10-15 mm are more likely to require intervention [704]. The initial approach to the ureter can be either intravesical, extravesical or combined. Several tailoring techniques exist, such as ureteral imbrication or excisional tapering [705]. Some institutions perform endoscopic stenting, but there is still no long-term data and no prospective randomised trials to confirm their outcome. Meticulous and repeat postnatal evaluation is mandatory to try to identify obstructive cases at risk of renal deterioration and requiring surgical reconstruction. Ureteropelvic junction obstruction is the leading cause of hydronephrotic kidneys (40%). Offer continuous antibiotic prophylaxis to the subgroup of children with antenatal 2 Weak hydronephrosis who are at high risk of developing urinary tract infection like uncircumcised infants, children diagnosed with hydroureteronephrosis and high grade hydronephrosis, respectively. Decide on surgical intervention based on the time course of the hydronephrosis 2 Weak and the impairment of renal function. Offer pyeloplasty when ureteropelvic junction obstruction has been confirmed 2 Weak clinically or with serial imaging studies proving a substantially impaired or decrease in function. Do not offer surgery as a standard for primary megaureters since the spontaneous 2 Strong remission rates are as high as 85%. The scientific literature for reflux disease is still limited and the level of evidence is generally low. Most of the studies are retrospective, include different patient groups, and have poor stratification of quality. Also, there is a high risk of presenting misleading results by combining different types of studies when systematically extracting data. Therefore, for reflux disease, it is unfortunately not possible to produce recommendations based on high-quality studies. The authors have assessed the current literature, but in the absence of conclusive findings, have provided recommendations based on panel consensus. Vesicoureteric reflux is a very common urological anomaly in children, with an incidence of nearly 1%. The main management goal is the preservation of kidney function, by minimising the risk of pyelonephritis. Urinary tract infections are more common in girls than boys due to anatomical differences. Renal scarring may adversely affect renal growth and function, with bilateral scarring increasing the risk of insufficiency. Dimercaptosuccinic acid is taken up by proximal renal tubular cells and is a good indicator of renal parenchyma function. Dimercaptosuccinic acid scans are therefore used to detect and monitor renal scarring. Dimercaptosuccinic acid can also be used as a diagnostic tool during suspected episodes of acute pyelonephritis [744]. Cystoscopy has a limited role in evaluating reflux, except for infravesical obstruction or ureteral anomalies that might influence therapy. It is non-invasive and provides reliable information regarding kidney structure, size, parenchymal thickness and collecting system dilatation [745, 746]. Ultrasound should be delayed until the first week after birth because of early oliguria in the neonate. Patients with severe hydronephrosis and those whose hydronephrosis is sustained or progressive, need further evaluation to exclude obstruction. Conservative management should be dismissed in all cases of febrile breakthrough infections, despite prophylaxis, and intervention should be considered. It is clear that antibiotic prophylaxis may not be needed in every reflux patient [732, 762-764]. It is strongly advised that the advantages and disadvantages should be discussed in detail with the family. Using cystoscopy, a bulking material is injected beneath the intramural part of the ureter in a submucosal location. The injected bulking agent elevates the ureteral orifice and the distal ureter, so that coaptation is increased. This results in narrowing of the lumen, which prevents reflux of urine into the ureter, while still allowing its antegrade flow. Although they are all biocompatible, other compounds such as collagen and chondrocytes have failed to provide a good outcome. Initial clinical trials have demonstrated that this method is effective in treating reflux [774]. Studies with long-term follow-up have shown that there is a high recurrence rate which may reach as high as 20% in two years [762]. If the first injection was unsuccessful, the second treatment had a success rate of 68% and the third treatment 34%. Clinical validation of the effectiveness of anti-reflux endoscopy is currently hampered by the lack of methodologically appropriate studies. New scar formation rate was higher with endoscopic injection (7%) compared with antibiotic prophylaxis (0%) [776]. Although different methods have specific advantages and complications, they all share the basic principle of lengthening the intramural part of the ureter by submucosal embedding of the ureter. All techniques have been shown to be safe with a low rate of complications and excellent success rates (92-98%) [777]. The most popular and reliable open procedure is cross trigonal re-implantation described by Cohen. The main concern with this procedure is the difficulty of accessing the ureters endoscopically if needed when the child is older. Alternatives are suprahiatal re-implantation (Politano-Leadbetter technique) and infrahiatal re-implantation (Glenn-Anderson technique). If an extravesical procedure (Lich-Gregoir) is planned, cystoscopy should be performed pre-operatively to assess the bladder mucosa and the position and configuration of the ureteric orifices. In bilateral reflux, an intravesical anti-reflux procedure may be considered, because simultaneous bilateral extravesical reflux repair carries an increased risk of temporary post-operative urine retention [778]. Various anti-reflux surgeries have been performed with the robot and the extravesical approach is the most commonly used. Although initial reports give comparable outcomes to their open surgical counterparts in terms of successful resolution of reflux, further studies are needed to define the success rates, costs and benefits of this minimal invasive approach [779, 780]. The major shortcoming of the new techniques seems to be the longer operative times, which hinder their wider acceptance. Also, laparoscopic or robotic assisted approaches are more invasive than endoscopic correction and their advantages over open surgery are still debated. Therefore, at present, a laparoscopic approach cannot be recommended as a routine procedure. It can be offered as an alternative to the caregivers in centres where there is established experience [761, 780-788]. The traditional approach of initial medical treatment after diagnosis and shifting to interventional treatment in case of breakthrough infections and new scar formation needs to be challenged, because the treatment should be tailored to different risk groups. The outcome of open surgical correction is better than endoscopic correction for higher grades of reflux, whereas satisfactory results can be achieved by endoscopic injection for lower grades. The choice of management depends on the presence of renal scars, clinical course, grade of reflux, ipsilateral renal function, bilaterality, bladder function, associated anomalies of the urinary tract, age, compliance, and parental preference. Offer immediate, parenteral antibiotic treatment for febrile breakthrough infections. Strong Offer definitive surgical or endoscopic correction to patients with frequent breakthrough Weak infections. Offer open surgical correction to patients with persistent high-grade reflux and Strong endoscopic correction for lower grades of reflux. Strong Offer surgical repair to children above the age of one presenting with high-grade reflux and Weak abnormal renal parenchyma. Offer close surveillance without antibiotic prophylaxis to children presenting with lower Strong grades of reflux and without symptoms. Offer surgical correction, if parents prefer definitive therapy to conservative management. In high-risk patients who already have renal impairment, a more aggressive, Strong multidisciplinary approach is needed. Due to its recurrent nature, every effort should be made to discover the underlying metabolic abnormality so that it can be treated appropriately. Obtaining a stone-free state with close follow-up are of the utmost importance, although, it may not be possible in some circumstances. Bladder stones are still common in underdeveloped areas of the world and are usually ammonium acid urate and uric acid stones, strongly implicating dietary factors [789]. Patients with augmented bladder constitute another important group with a risk of up to 15% [790]. The incidence and characteristics of stones show a wide geographical variation in children. Although urinary stone disease is generally considered to be a relatively rare disease, it is quite common in some parts of the world. Paediatric stone disease is endemic in Turkey, Pakistan and in some South Asian, African and South American states. However, recent epidemiological studies have shown that the incidence of paediatric stone disease is also increasing in the Western world [791-793], especially in girls, Caucasian ethnicity, African Americans and older children [794]. More than 70% of stones in children contain calcium oxalate, while infection stones are found more frequently in younger children [795]. Super-saturation of calcium (hypercalciuria) and oxalate (hyperoxaluria) or decreased concentration of inhibitors, such as citrate (hypocitraturia) or magnesium (hypomagnesemia) play a major role in the formation of calcium oxalate stones. Hypercalciuria: this is defined by a 24-hour urinary calcium excretion of more than 4 mg/kg/day (0. Idiopathic hypercalciuria is diagnosed when clinical, laboratory, and radiographic investigations fail to delineate an underlying cause leading to hypercalcaemia. Secondary hypercalciuria occurs when a known process produces excessive urinary calcium. In secondary (hypercalcemic) hypercalciuria, a high serum calcium level may be due to increased bone resorption (hyperparathyroidism, hyperthyroidism, immobilisation, acidosis, metastatic disease) or gastrointestinal hyperabsorption (hypervitaminosis D) [797]. A good screening test for hypercalciuria compares the ratio of urinary calcium to creatinine. Neonates and infants have a higher calcium excretion and lower creatinine excretion than older children [796, 797]. If the follow-up ratios are normal, then no additional testing for hypercalciuria is needed. However, if the ratio remains elevated, a timed 24-hour urine collection should be obtained and the calcium excretion calculated. The 24-hour calcium excretion test is the standard criterion for the diagnosis of hypercalciuria. In addition to calcium, the 24-hour urine analysis should also include phosphorus, sodium, magnesium, uric acid, citrate and oxalate. The child should be referred to a dietician to assess accurately the daily intake of calcium, animal protein, and sodium. Dietary sodium restriction is recommended as well as maintenance of calcium intake consistent with the daily needs of the child [800]. A brief trial of a low calcium diet can be carried out to determine if exogenous calcium intake and/or calcium hyperabsorption is contributing to high urinary calcium.
Order suhagra uk. Treatment for Erectile Dysfunction: Mayo Clinic Radio.